Five key behavioral red flags can help you identify potential addiction: social withdrawal from family and friends, neglect of personal and professional responsibilities, unpredictable emotional changes including mood swings and irritability, engagement in high-risk activities despite negative consequences, and physical signs like changes in sleep patterns or hygiene. Understanding these warning signs enables early intervention, and recognizing these patterns marks the first step toward addressing underlying substance abuse issues.
Withdrawal From Social Life and Relationships

While behavioral addiction manifests in various ways, withdrawal from social life and relationships stands as one of its most telling indicators. You’ll notice a steady decline in meaningful social connections, as individuals with addictive behaviors often retreat from friends, family, and community engagement. A concerning statistic reveals that 2.3% of adults screen positive for social media addiction, highlighting the prevalence of this issue.
This social isolation typically coincides with heightened emotional loneliness, affecting multiple relationship dimensions – from intimate partnerships to familial bonds. Studies show that young single women are particularly vulnerable to this type of withdrawal and addiction. You’ll observe a concerning pattern where face-to-face interactions are replaced with virtual connections or solitary activities, leading to superficial relationships that fail to provide genuine intimacy. The withdrawal cycle intensifies as mental health deteriorates, with increased rates of depression and anxiety further fueling social avoidance. Research indicates that prolonged isolation lasting three or more years significantly increases depression risk. This creates a destructive loop where isolation and addiction reinforce each other, making intervention essential for recovery.
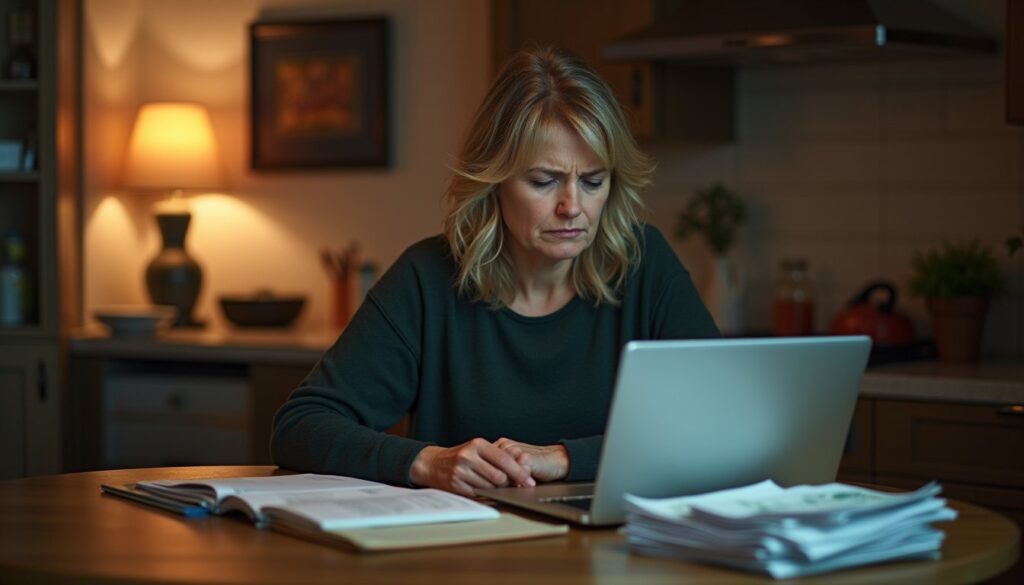
Neglecting Personal and Professional Duties
When addiction takes hold, neglect of personal and professional duties emerges as a prominent warning sign that demands attention. You’ll notice a significant decline in job performance, with tasks left incomplete and deadlines missed. Your once-stable life routines begin to crumble as basic responsibilities fall by the wayside. Poor mental health often accelerates this pattern of neglect, making recovery more challenging without proper intervention. Understanding that compulsive behavior patterns drive these changes helps explain why individuals struggle to maintain their responsibilities despite wanting to do better. Studies show that high relapse rates occur within the first year of recovery, making sustained support crucial for overcoming these challenges.
- Your workplace reliability deteriorates, marked by increased absenteeism, missed meetings, and mounting disciplinary actions from supervisors
- Basic household chores and self-care routines become overlooked, resulting in unkempt living spaces and poor personal hygiene
- Financial obligations suffer as spending priorities shift toward feeding the addiction, leading to mounting debts and possible legal consequences
- Academic or professional development stalls, characterized by missed classes, declining grades, or reduced engagement in career advancement opportunities
Unpredictable Emotional Changes

Throughout the progression of addiction, unpredictable emotional changes emerge as telltale indicators of substance dependence’s grip on the brain. You’ll notice dramatic mood fluctuations, where moments of euphoria rapidly shift to intense sadness or irritability. This emotional dysregulation manifests through disproportionate reactions to minor stressors and frequent episodes of anxiety, anger, or paranoia. Individuals experiencing these symptoms often demonstrate compulsive drug use to alleviate their negative emotional states. Family members watching these transformations may develop anxiety and worry about their loved one’s well-being.
You might experience periods of complete emotional numbness, finding it difficult to connect with others or feel joy in previously pleasurable activities. These changes often coincide with deep-seated feelings of shame and guilt, creating a cycle that reinforces addictive behaviors. Your ability to regulate emotions becomes increasingly compromised as the addiction affects brain regions responsible for emotional control, leading to impulsive decisions even when you’re aware of negative consequences. In fact, chemical imbalances caused by prolonged substance use significantly contribute to these severe mood disturbances and emotional instability.
Engaging in High-Risk Activities
As addiction progresses, individuals frequently engage in increasingly dangerous behaviors that jeopardize their safety and wellbeing. This extreme thrill seeking often stems from impaired decision making, leading to activities that put both themselves and others at serious risk. The person may display sudden mood swings and become increasingly volatile when confronted about their risky actions. Having access to extra disposable income can intensify these dangerous patterns of behavior. Mental health disorders often contribute to these risky behaviors as individuals attempt to self-medicate through substance use.
- Engaging in dangerous activities like driving under the influence, operating heavy machinery while intoxicated, or participating in unsafe sexual practices
- Seeking out high-risk environments and associating with individuals who encourage risky substance use
- Disregarding personal safety protocols and professional obligations, resulting in accidents, injuries, or job loss
- Making reckless financial decisions, including gambling large sums of money or selling personal belongings to maintain substance use
These behaviors typically escalate as tolerance increases, creating a dangerous cycle that can result in legal troubles, physical harm, or severe financial consequences.
Physical Signs of Substance Use
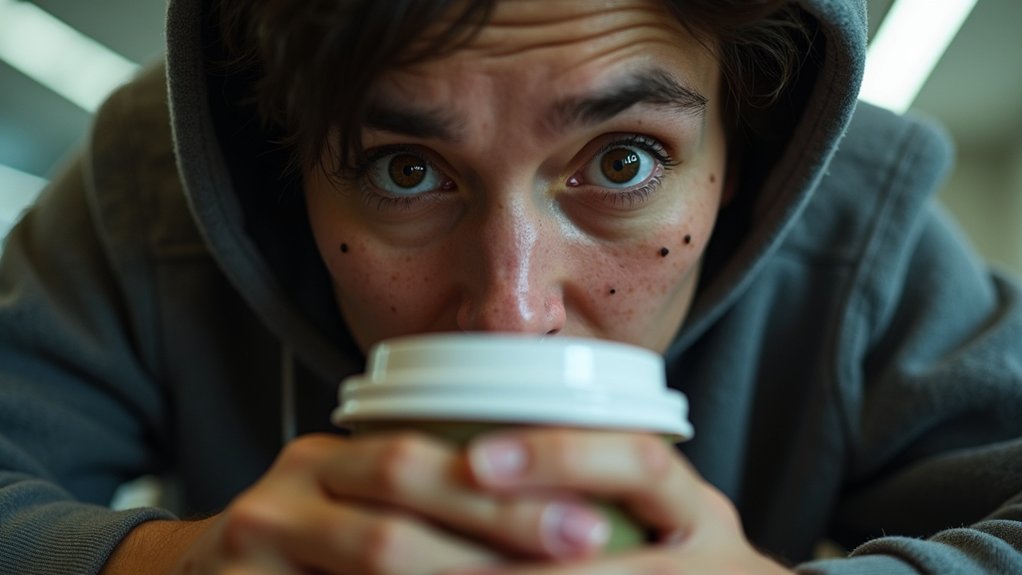
The physical manifestation of substance use disorders presents through five key indicators that medical professionals and concerned individuals should monitor. You’ll notice changes ranging from bloodshot eyes and pupil irregularities to significant weight fluctuations and deteriorating hygiene. Security measures help protect sensitive medical information when tracking these symptoms online.
| Physical Sign | Primary Indicators | Common Substances |
|---|---|---|
| Eye Changes | Redness, pupil dilation | Stimulants, cannabis |
| Weight Changes | Rapid loss or gain | Amphetamines, opioids |
| Hygiene Decline | Unkempt appearance | Multiple substances |
Watch for disrupted sleep patterns, including insomnia or excessive drowsiness, which often indicate substance abuse. You’ll also observe impaired coordination, manifesting as slurred speech, poor balance, or unsteady movements. These physical signs typically worsen as substance use progresses, making early recognition vital for intervention.
Frequently Asked Questions
How Long After Quitting Substances Do Behavioral Changes Typically Return to Normal?
You’ll experience significant behavioral improvements over a 6-12 month timeline, though withdrawal symptoms initially intensify behavioral disruptions. While early recovery (1-3 months) shows gradual improvements, your brain needs at least 6 months to establish stable behavioral patterns. Your recovery timeline varies based on substance type and usage duration, but you’ll typically achieve behavioral normalization within a year if you maintain consistent therapeutic support and healthy habits.
Can Addiction-Related Behavioral Changes Be Permanent Even After Achieving Sobriety?
Yes, addiction-related behavioral changes can become permanent if you don’t actively address them during your recovery journey. The long term effects on your brain’s reward and executive function circuits can persist indefinitely, even after achieving sobriety. You’ll need extensive behavioral therapy and ongoing support to reverse these changes. Without proper intervention, you may continue struggling with maladaptive patterns, emotional dysregulation, and trigger responses despite maintaining abstinence.
What Percentage of People Displaying These Red Flags Actually Have Addiction?
Based on thorough addiction statistics, you can expect around 33% of people showing behavioral red flags to actually have a diagnosable addiction. While you’ll notice these warning signs in many individuals, only one-quarter to one-third meet clinical diagnostic criteria. The prevalence varies greatly by addiction type, from gambling’s 1-2.7% to social media’s 8-15%. Remember that displaying red flags alone isn’t sufficient for diagnosis; you’ll need a thorough clinical assessment.
At What Age Do Behavioral Red Flags Most Commonly First Appear?
You’ll typically see behavioral red flags first emerge during early to mid-adolescence, primarily between ages 12-17. Early warning signs become most prominent around ages 13-15, coinciding with significant social and developmental changes. The teenage onset of these indicators often manifests through sudden mood swings, social withdrawal, and academic decline. You should pay particular attention to the critical risk period of ages 11-14, when these warning signs frequently begin clustering together.
How Do Behavioral Red Flags Differ Between Men and Women With Addiction?
You’ll notice distinct gender differences in addiction warning signs. Women typically show higher impulsivity, more intense emotional distress, and greater self-medication tendencies. Men exhibit more social risk-taking and group-based substance use behaviors. For effective addiction awareness, watch for women’s rapid escalation of use and comorbid mental health issues, while men often display more stable usage patterns but stronger physical withdrawal symptoms. Women seek help earlier but face unique barriers like childcare concerns.