Alcohol and antidepressants are two of the most widely used and common substances in the United States; many people forget that both have dangerous side effects, and even fewer people know the dangers of combining alcohol and antidepressants.
Many people drink to cope with depression, believing that once their depression is under control with medications, drinking won’t be as much of an issue. In reality, whether you drink socially, drink regularly, or struggle with alcohol use disorder, there is no safe amount of alcohol to mix with antidepressants.
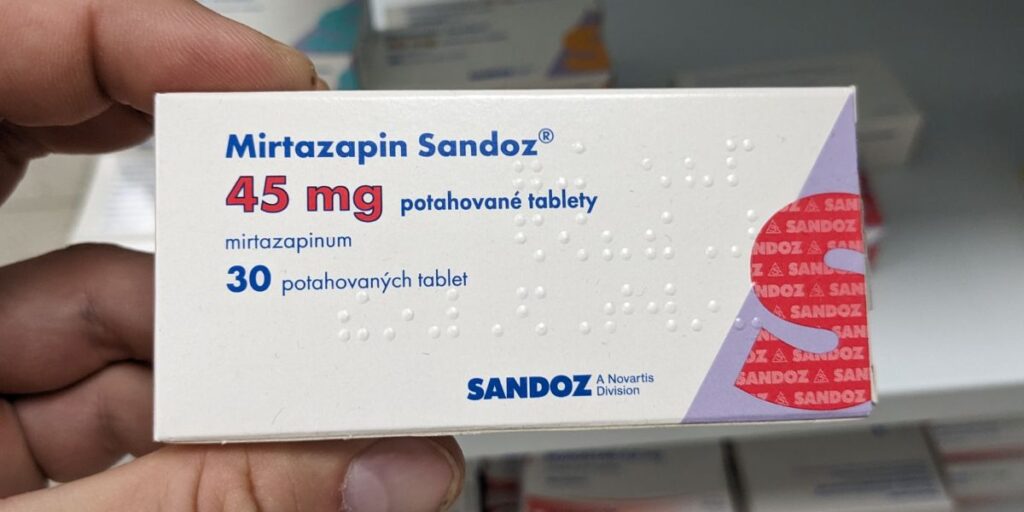
What Are Antidepressants?
Antidepressants are prescription medications that treat depression, mood disorders, and various associated conditions. Antidepressants help correct or improve the chemical balance in the brain to improve or eliminate mental illness symptoms.
Antidepressants have a cumulative effect, meaning you must take them regularly to be effective; quitting them requires medical supervision and careful tapering to avoid harmful side effects.
Classes of Antidepressants
Different classes of antidepressants exist to treat various mental health conditions. The three main types of antidepressants are separated by how they affect the brain and the specific chemicals. Over time, some people become tolerant of different kinds of antidepressants and need to switch to continue to benefit from them.
The three main classes of antidepressants include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs work with neurotransmitters to help prevent the body from absorbing serotonin too quickly, keeping it in the brain longer, reducing depression, and improving focus and memory.
Monoamine Oxidase Inhibitors (MAOIs)
MAOIs affect specific enzymes, preventing them from breaking down serotonin, norepinephrine, and dopamine too quickly, reducing depression and anxiety.
Tricyclic Antidepressants (TCAs)
TCAs affect neurotransmitters to help regulate how long serotonin and norepinephrine stay in the system, reducing depression and improving mood regulation.
What Happens When You Mix Alcohol and Antidepressants?
When you mix alcohol and antidepressants, the chemical reactions reduce the effectiveness of the medications and can even worsen symptoms of depression.
Both antidepressants and alcohol cause dizziness, drowsiness, and impaired motor function, even at low blood alcohol levels. Mixing alcohol and antidepressants can drastically increase those effects, making driving or operating machinery and other activities dangerous.
Furthermore, many of the neurotransmitters and organs responsible for processing antidepressants also metabolize alcohol; the presence of both substances at the same time can overload the body, causing an increased risk of alcohol poisoning.
Drinking alcohol while on antidepressants called monoamine oxidase inhibitors (MAOIs) can cause dangerous spikes in blood pressure, which can be fatal.
How Much Alcohol Can You Drink While on Antidepressants?
The National Alliance on Mental Illness (NAMI) strongly advises against drinking while taking antidepressants and clarifies that if you insist on having alcohol, you should wait until you are sure how your antidepressant affects you.
If you are planning to drink alcohol while on antidepressants, NAMI advises doing so with food and water and sticking to moderate drinking. The accepted definition of moderate drinking is one drink a day for adult women or two drinks for adult men.
A standard drink is:
- 12 oz of beer
- 5 oz of wine
- 1.5 oz of hard liquor
Even if you only have one drink while on antidepressants, you should avoid driving or operating heavy machinery out of an abundance of safety.
People who binge drink or consider themselves functioning alcoholics often believe they are immune to the side effects of mixing alcohol and antidepressants, especially if they don’t drink daily. The reality is that they may be better at masking the immediate results; however, they still have an increased risk for dangerous and long-term health conditions.

Side Effects of Combining Antidepressants
The side effects of combining antidepressants and alcohol and resulting interactions will vary based on physical makeup, the type of antidepressant, and how much alcohol they consume.
Common side effects when people combine alcohol and antidepressants include:
- Dizziness
- Drowsiness
- Memory loss
- Lack of coordination
- Headache
- Nausea
- Vomiting
- Poor judgment
- Dangerous spikes in blood pressure
- Confusion
- Seizures
- Alcohol poisoning
- Suicidal thoughts
- Serotonin syndrome, an overactivation of brain receptors
Repeatedly combining alcohol and antidepressants also increases the risks of:
- Developing substance use disorders
- Blood clots
- Stroke
- Alcohol withdrawal syndrome (AWS)
- Liver damage
- Memory impairment
- Heart damage
- Sexual dysfunction
- Genetic abnormalities in children
- Suicide
Worsens Depression
Research has shown that drinking on antidepressants typically worsens symptoms of depression at an accelerated rate. Depressed people engage in substance abuse at higher rates than non-depressed people and people undergoing treatment programs for depression and anxiety.
People who binge drink regularly are twice as likely to have suicidal thoughts, and 1 in 4 people who commit suicide have a blood alcohol content over .08%, according to the National Institute on Alcohol Abuse and Alcoholism (NIAA).
Depressive disorders are the most commonly diagnosed mental health conditions in people with substance use disorders. Alcohol reduces the effectiveness of antidepressants, and people are less likely to stick to a medication routine when regularly drinking.
Many people struggling with alcohol abuse need professional help to stop drinking. Integrated treatment facilities and programs licensed to handle mental health conditions and substance use disorders are the most effective option for treating co-occurring conditions.

Substance Use Disorder Treatment
If you struggle with substance abuse and mental health, you don’t have to suffer alone. At Northridge Addiction Treatment Center, we know how hard it can be to feel like you’re fighting a losing battle. We take an evidence-based, whole-person approach to treat all aspects of your addiction, not just the symptoms.
Our onsite medical detox provides 24-hour care and support from licensed medical professionals to ensure that you stay safe while your body rids itself of harmful substances.
We use medication-assisted treatment to evaluate and adjust any medications you need for mental health conditions while using heavily researched and scientifically backed therapies to address your addiction’s roots and behavioral aspects.
The path to a healthy life in recovery is a phone call away. Reach out to our team of expert treatment specialists now.