Modern addiction treatment offers you multiple evidence-based approaches, combining FDA-approved medications with behavioral therapies for ideal outcomes. You’ll find traditional methods like medication-assisted treatments using methadone or buprenorphine, alongside advanced options including trauma-informed care, digital health monitoring, and telehealth services. Treatment success rates increase by 35% when practitioners integrate multiple modalities into your personalized plan. The expanding field of addiction medicine continues to evolve with promising technological and therapeutic innovations.
Evidence-Based Medical Treatments and Interventions

While addiction treatment has evolved considerably over the decades, evidence-based medical interventions now form the cornerstone of modern substance use disorder care. Evidence-based practices incorporate both FDA-approved medications and structured behavioral therapies to address substance dependence thoroughly. Due to security measures in place, some treatment information websites may temporarily restrict access to protect sensitive content. Treatment engagement duration plays a key role, as longer participation periods correlate with improved recovery outcomes.
Medication-assisted treatment options include methadone and buprenorphine for opioid use disorder, while naltrexone helps combat both opioid and alcohol dependencies. For alcohol use disorder specifically, you’ll find acamprosate reducing cravings and disulfiram creating aversion responses. These pharmaceuticals work alongside behavioral interventions like cognitive-behavioral therapy and contingency management to modify maladaptive patterns. Your treatment plan may combine several approaches, as research shows integrated medication and behavioral therapy typically yields better outcomes than either method alone. Medical professionals provide around-the-clock supervision during the critical detoxification phase to ensure patient safety and comfort.
Advanced Therapeutic Modalities in Addiction Recovery
As addiction treatment continues to evolve, advanced therapeutic modalities now extend beyond traditional approaches to incorporate trauma-informed care, neurofeedback technologies, and holistic interventions. You’ll find evidence-based programs integrating mindfulness practices and emotional regulation techniques alongside cutting-edge treatments like psychedelic-assisted therapy and personalized AI-driven protocols. Strategic implementation of medication for addiction treatment combined with behavioral interventions has demonstrated significant success in supporting long-term recovery outcomes. Virtual recovery platforms are increasingly becoming essential components of comprehensive treatment programs, especially for those in remote areas. The emphasis on empathy and compassion has become fundamental in reinforcing successful healing processes. These advanced approaches target addiction’s complex nature through multiple pathways, combining physiological monitoring, biochemical restoration, and psychological healing to optimize treatment outcomes and reduce relapse risks.
| Modality | Primary Focus | Key Benefits |
|---|---|---|
| Trauma-Informed Care | Past Trauma Processing | Enhanced Recovery Rates |
| Neurofeedback | Neural Pathway Retraining | Improved Self-Regulation |
| Holistic Therapy | Mind-Body Integration | Extensive Healing |
| Psychedelic-Assisted | Pattern Disruption | Increased Self-Awareness |
| Personalized Recovery | Individual Adaptation | Targeted Outcomes |
Technology-Driven Solutions for Addiction Treatment

Modern digital health monitoring systems equip you with real-time tracking of physiological markers and behavioral patterns through integrated wearable devices and mobile applications. You’ll benefit from continuous data collection that enables healthcare providers to detect early warning signs of potential relapse and implement timely interventions through AI-driven analytics. Remote treatment accessibility expands your care options through virtual platforms, offering 24/7 support, telehealth sessions, and digital therapeutic tools that complement traditional in-person treatment methods. The implementation of personalized treatment plans has revolutionized addiction recovery by utilizing data-driven insights to create more effective and individualized care strategies. These technological solutions help address the critical gap in treatment access, considering that less than 10% of individuals with substance use disorders currently receive the care they need. Virtual reality technology provides exposure therapy environments where patients can safely confront and manage their triggers under professional guidance.
Digital Health Monitoring Systems
Technology-driven solutions have revolutionized addiction treatment through sophisticated digital health monitoring systems. You’ll find AI monitoring and wearable technology at the forefront, enabling real-time analysis of physiological changes that predict relapse risks. These systems integrate seamlessly with cloud-based platforms, allowing your care team to monitor essential signs and intervene proactively. Studies show that patients using these digital solutions achieve 72.5% compliance rates with their care plan tasks. The introduction of telehealth services has significantly expanded access to treatment, particularly for patients in remote areas. The implementation of mobile health apps has enhanced patient education and ongoing support during recovery.
| Monitoring Feature | Clinical Benefit |
|---|---|
| Biometric tracking | Early detection of substance use patterns |
| Real-time analytics | Immediate intervention capabilities |
| Cloud integration | Enhanced care team coordination |
| Automated alerts | Proactive crisis prevention |
Through platforms like Biofourmis, you’ll receive continuous monitoring of essential signs, sleep patterns, and stress levels. The system’s predictive algorithms identify concerning trends before they escalate into critical incidents, while prescription monitoring systems prevent potential medication misuse, ensuring your recovery stays on track.
Remote Treatment Accessibility
Remote addiction treatment has evolved into an extensive digital ecosystem, revolutionizing accessibility for patients worldwide. Through virtual therapy platforms, you’ll find specialized apps that deliver counseling sessions, track your progress, and provide educational resources tailored to your recovery journey. With 15.6% of Americans needing substance use treatment annually, remote solutions have become increasingly vital. These digital solutions are particularly beneficial for outpatient treatment, which is offered by 82% of facilities nationwide. The rise of digital healthcare has transformed treatment delivery, with one in three rehabilitation appointments now conducted virtually.
You can access remote support through various channels, including telehealth services that reach previously underserved areas and demographics. AI-driven systems analyze your health metrics and behavioral patterns to customize treatment plans, while wearable devices monitor essential signs and trigger real-time interventions when needed. Cross-platform support systems enable continuous communication with peers and counselors through WhatsApp groups and video calls, ensuring you maintain connections throughout recovery. This technology-driven approach effectively reduces traditional barriers like travel costs, geographic limitations, and treatment stigma while offering cost-effective alternatives to residential care.
Trauma-Informed Care Approaches
While traditional addiction treatment often focuses solely on substance use, trauma-informed care approaches recognize the intricate relationship between past trauma and addiction development. This evidence-based framework emphasizes understanding how trauma triggers influence substance use, with research showing that over 75% of addiction cases link to unresolved trauma. Treatment providers ensure trustworthiness and boundaries through consistent and transparent care protocols.
You’ll find that effective trauma-informed treatment incorporates cultural sensitivity and prioritizes both physical and emotional safety. The approach shifts from asking “what’s wrong?” to “what happened to you?” while implementing nonviolent practices that minimize power imbalances. Treatment programs utilize prospective screening tools and integrated care models, combining addiction treatment with psychological support. This method has demonstrated improved patient engagement, reduced relapse rates, and enhanced long-term resilience without increasing treatment costs.
Holistic and Alternative Healing Methods

Beyond conventional treatment methods, holistic and alternative healing approaches offer extensive pathways for addiction recovery by addressing physical, emotional, and spiritual well-being simultaneously.
You’ll find art therapy and creative expression providing essential outlets for emotional processing, while mindfulness practices and therapeutic yoga enhance self-awareness and stress management. Energy healing methods like Reiki complement bodywork techniques such as massage therapy to promote physical and spiritual balance. Holistic nutrition and herbal remedies support your body’s natural healing processes during detoxification. Recreational activities, from hiking to horseback riding, help establish healthy routines while reducing anxiety. These evidence-based complementary approaches, now used by approximately 40% of U.S. adults, integrate effectively with traditional treatment models to create thorough recovery programs that target multiple aspects of healing.
Mind-Body Integration Techniques
Mind-body integration techniques represent a cornerstone of modern addiction treatment, merging evidence-based practices like mindfulness, meditation, and yoga therapy to address both physiological and psychological aspects of recovery.
You’ll find that mindfulness practices enhance your awareness of triggers while facilitating emotional processing through non-judgmental acceptance. The MORE program combines these approaches with positive psychology to reduce your reactivity to substance-related cues. Through guided meditation sessions and breathwork integration, you’ll develop stronger stress mitigation skills and emotional regulation capabilities.
Trauma-sensitive yoga therapy and restorative postures help rebuild your physical resilience while calming your nervous system. When combined with conventional treatments, these techniques show improved outcomes according to NIH evaluations, particularly when implemented through personalized assessments and gradual, collaborative care approaches.
Emerging Psychedelic-Assisted Therapies
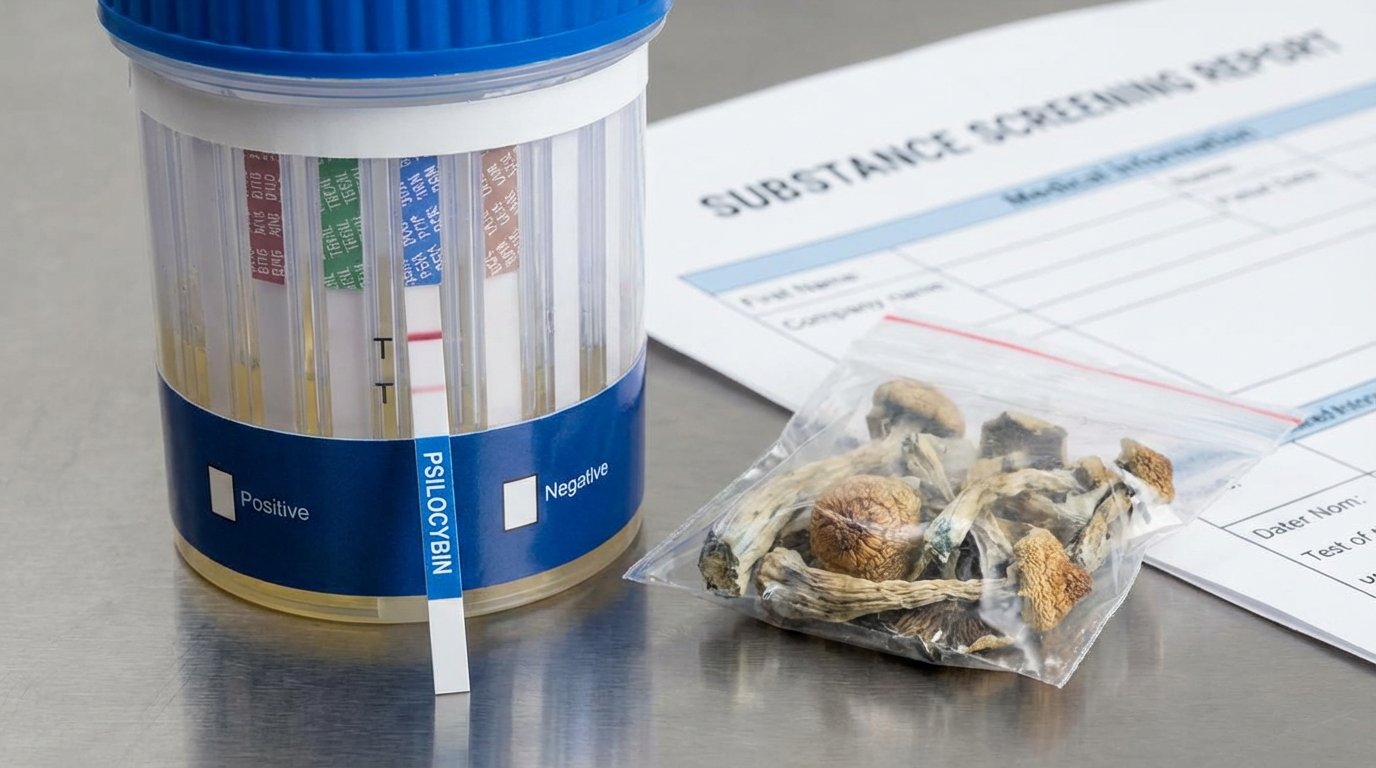
Psychedelic-assisted therapy represents a significant advancement in addiction treatment, with psilocybin showing particular promise for substance use disorders through its ability to promote neuroplasticity and reset entrenched behavioral patterns. You’ll find that MDMA‘s unique capacity to facilitate trauma processing makes it especially valuable for addressing the underlying psychological wounds often driving addiction. Clinical evidence indicates these compounds, when administered in controlled therapeutic settings, can help you achieve lasting recovery by enhancing emotional processing and strengthening therapeutic outcomes.
Psilocybin’s Role In Recovery
While traditional addiction treatments have shown mixed results, emerging research reveals psilocybin-assisted therapy as a promising intervention across multiple substance use disorders. You’ll find this approach particularly effective in treating alcohol dependence, opioid addiction, and smoking cessation, with clinical trials demonstrating sustained benefits in recovery outcomes.
The success of psilocybin therapy in addiction recovery stems from its unique mechanisms of action. It enhances neuroplasticity, disrupts rigid thought patterns in the default mode network, and creates lasting changes in hippocampal connectivity. When combined with cognitive behavioral therapy, you’ll see amplified therapeutic effects and improved retention of insights. Current research shows this treatment is remarkably safe when administered in controlled settings, with rigorous screening protocols ensuring patient safety. Most importantly, participants often achieve sustained improvements with just one or two supervised sessions.
MDMA For Trauma Healing
As PTSD treatment options have stagnated over two decades, MDMA-assisted therapy emerges as a groundbreaking intervention with FDA breakthrough status. You’ll find that MDMA therapy enhances neuroplasticity and emotional processing, allowing deeper engagement with traumatic memories during treatment sessions.
| Component | Duration | Outcome |
|---|---|---|
| Education | Pre-session | Treatment preparation |
| MDMA Administration | 6-8 hours | Enhanced emotional access |
| Prolonged Exposure | 2 weeks | Trauma processing |
| Integration | Ongoing | Symptom reduction |
Clinical trials demonstrate significant improvement, with CAPS-5 scores showing a 24-point reduction in PTSD severity compared to 13-14 points with placebo. The protocol combines supervised MDMA sessions with intensive prolonged exposure therapy, maximizing therapeutic benefits. Current research, supported by a $4.9 million DoD grant, prioritizes military and veteran populations, addressing critical treatment gaps in these high-risk groups.
Digital Health and Remote Treatment Options
Recent advances in digital health technologies have revolutionized addiction treatment delivery, enabling remote care options that maximize accessibility and effectiveness. You’ll find evidence-based digital therapeutics achieving over 70% remission rates, while structured digital detox programs demonstrate 72% success in reducing compulsive technology use.
These platforms integrate AI-driven monitoring through wearable devices, tracking your physiological markers in real-time. You can access virtual communities through WhatsApp groups, providing immediate peer support and clinical guidance. Treatment personalization occurs through adaptive platforms that adjust therapy intensity based on your individual responses. The integration of telehealth services with traditional healthcare records guarantees thorough care coordination, while real-time analytics dashboards help clinicians optimize your treatment protocol. This digital transformation enables ten times more patients to receive evidence-based addiction treatment.
Personalized Treatment Protocols and Monitoring Systems
Because successful addiction treatment requires individualized approaches, personalized protocols now incorporate thorough assessment metrics across multiple domains. These personalized assessments evaluate your genetic factors, mental health status, trauma history, and substance use patterns to determine ideal treatment intensity and modality selection.
Through adaptive strategies, your treatment team continuously monitors progress using biomarker testing, predictive analytics, and regular reassessments. This data-driven approach allows for real-time adjustments to your care plan, with studies showing up to 33% difference in abstinence rates between matched and mismatched treatments. Your protocol might combine cognitive-behavioral therapy, medication-assisted treatment, and culturally adapted interventions based on your specific needs. For dual diagnoses, integrated care coordinates treatment across multiple specialists, addressing both addiction and co-occurring mental health conditions simultaneously.
Frequently Asked Questions
How Long Does It Typically Take to Fully Recover From Addiction?
Recovery timelines vary greatly based on multiple duration factors. You’ll find that 75% of individuals eventually achieve recovery, though the path differs by substance opioid users typically resolve addiction in 8.4 years, while alcohol use disorder often spans decades. Your recovery journey requires ongoing support, with most people needing multiple attempts before achieving stable sobriety. Success rates at one year post-treatment range from 29-41%, depending on the substance used.
What Percentage of People Relapse After Completing Addiction Treatment Programs?
You’ll find that relapse rates after addiction treatment are significant, with 40-60% of individuals returning to substance use, similar to other chronic conditions. Within the first year post-treatment, approximately 85% of people experience a relapse, with two-thirds occurring in the initial weeks. Treatment effectiveness varies by substance: opioids show up to 91% relapse rates, alcohol ranges from 40-80%, and stimulants average 50% in the first year.
Are Addiction Treatment Programs Covered by Most Insurance Plans?
Yes, you’ll find that most insurance plans now cover addiction treatment, thanks to mental health parity laws. Medicare, Medicaid, and ACA-compliant plans must include coverage for substance use disorder treatment. Treatment affordability has improved with 72% of providers accepting Medicaid and 42% accepting Medicare. However, your specific insurance coverage levels, out-of-pocket costs, and provider network options will vary based on your plan type and location.
Can Someone Be Forced Into Addiction Treatment Against Their Will?
Yes, you can be forced into addiction treatment against your will through involuntary treatment laws, which exist in 37 states and DC. The legal implications vary by state, with different requirements for who can petition for commitment and how long you can be held. However, research shows mixed results on effectiveness, with some studies indicating increased overdose risks post-release. Court-ordered treatment typically ranges from 1 day to 1 year, depending on jurisdiction.
What Role Do Genetics Play in Addiction Susceptibility and Treatment Success?
Your genetic predisposition greatly influences your addiction susceptibility, with about 50% of your risk linked to inherited factors. You’ll find specific genes, particularly those affecting dopamine and opioid pathways, play essential roles in how you respond to substances. These genetic variations also impact your treatment outcomes for instance, if you carry certain DRD2 or OPRM1 variants, you might respond differently to standard medications, potentially requiring personalized therapeutic approaches for best success.